|
DEPARTMENT
RESULTS |
|
|
| |
|
Goal:
Improve public health care program value |
|
Why is this goal
important?
 Rising health care costs are a serious problem. While there is no magic
bullet to make the problem go away, the Minnesota Department of Human
Services (DHS) is looking at a number of initiatives that will reduce costs
in both the short and long term. Rising health care costs are a serious problem. While there is no magic
bullet to make the problem go away, the Minnesota Department of Human
Services (DHS) is looking at a number of initiatives that will reduce costs
in both the short and long term.
In addition to the initiatives outlined below, DHS is taking steps to
improve program integrity and efficiency. This means making sure that
eligible Minnesotans
— and only those eligible
— are able to enroll in
Minnesota Health Care Programs (MHCP). It also involves automating the
current enrollment process to ensure that consistent guidelines are followed
when adding or retaining individuals in MHCP.
Basic health care costs account for approximately 49 percent of DHS’ state
funding. Costs include items such as hospital, physician, health maintenance
organizations (HMO) payments, etc., but not long-term care costs such as
nursing facilities. At a time of lean budgets, it is critical that DHS look
at all possible measures to reduce costs.
 |
 |
|
|
How
will this goal be accomplished?
DHS is pursuing several initiatives, including:
·
Prescription medication. DHS has implemented several cost-saving
initiatives, such as efforts to promote the use of generic medications. In
fall of 2004, DHS joined seven other states in a National Medicaid Pooling
Initiative (NMPI) to strengthen its ability to negotiate supplemental
rebates with drug companies. DHS participates in another multi-state program
called the Drug Effectiveness Review Project. The comprehensive drug reviews
produced by the project are used with NMPI rebate information to
establish a preferred drug list (a list of cost-effective drugs that can be
prescribed to MHCP recipients without restrictions). Doctors must get
approval before payment will be made for drugs not on the preferred drug
list.
·
Covered services. DHS completed the Health Care Services Study, as
requested by the 2003 Legislature to identify strategies to cut costs and
improve value in Minnesota Health Care Programs. The study was conducted
over 14 months and included input from enrollees, stakeholders, health care
providers, and national health care experts. The study also included an
independent review of Minnesota’s and other states’ practices for covering
health care services. The most viable of the identified strategies helped
form the basis for proposals presented to the 2005 Legislature related to
coverage policies, pharmacy purchasing. and medical care management for
chronically ill enrollees. Other strategies require further study and can be
pursued over time. The study is available
at
http://www.dhs.state.mn.us/healthcare/studies.
·
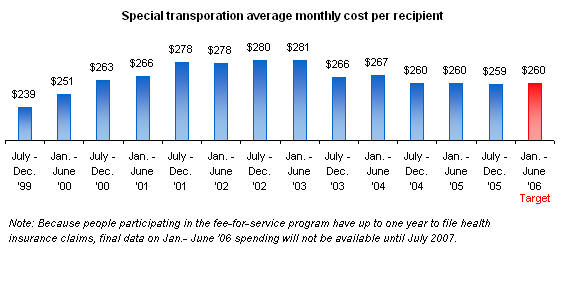
Special transportation. The department has been concerned for a number of
years about the lack of coordination of transportation to medical
appointments in the Twin Cities for health care program enrollees. These
concerns include the escalating costs of “special transportation” and the
difficulty in obtaining common carrier transportation such as bus or taxi.
To address these cost issues, the 2003 Legislature passed a number of
changes that affect non-emergency transportation, including the
implementation of a transportation coordinator within the seven-county metro
area. DHS contracted with Medical Transportation Management, Inc. in July
2004. This coordinator is responsible for authorizing appropriate levels of
transportation and managing common carrier transportation for enrollees who
need a ride to their medical appointments.
·
Disease management. Over the past several years, private sector health
plans have been focusing on disease management as a tool to manage their
enrollees’ health care and reduce costs. With MHCP, many MA enrollees who
are in fee-for-service plans are people with disabilities who have chronic
heath conditions. DHS is developing a
disease management pilot project where MA enrollees, on a voluntary basis,
would be assigned a nurse counselor who would manage the enrollee’s health
care needs. By providing individual professional care to enrollees, disease
management can ensure that enrollees are getting the necessary care when
they need it, thus avoiding emergency treatment, hospitalization or
longer-term care costs.
How
is DHS’ progress?
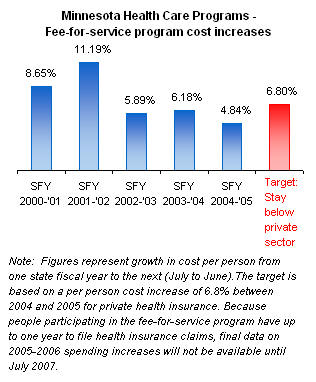
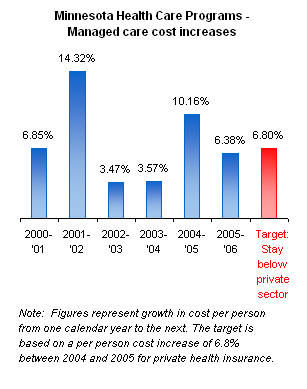
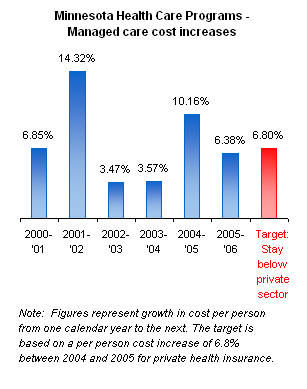
The cost per person in the fee-for-service portion of the Minnesota Health
Care Programs (MHCP) grew by 4.84 percent in 2005. Growth in the annual cost
per person in the managed care portion of MHCP was 6.38 percent in 2006.
DHS’ goal is to have spending on public programs grow at a rate slower than
the statewide private health insurance average, which was 6.8 percent for 2005.
The most recently measured average
monthly cost per recipient for prescriptions in MHCP was $268 for the last
half of 2005.
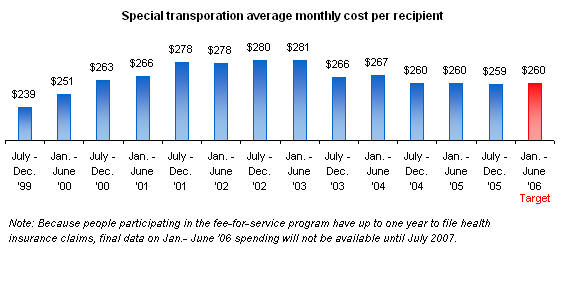
The most recently measured average monthly cost
per recipient for special transportation in MHCP was $259 for the last half
of 2005.
DHS’ goal for both of these costs is to reduce the historical growth
rate.
DHS is meeting its
targets as a result of improved management of services and, in part, due to
changes in payment policy. |
|
|
|
Goal:
Older Minnesotans will receive the long-term care services they need in
their homes and communities, will be able to choose how they receive
services, and will have more options for using their personal resources to
pay for long-term care |
|
Why
is this goal important?
Fueled by the aging of the baby boom generation, a much larger proportion
of the population than ever before will need long-term care over the next 30
years.
 As the major payer of long-term care services, the state could be
overwhelmed by the cost of long-term care for these elderly baby boomers. As the major payer of long-term care services, the state could be
overwhelmed by the cost of long-term care for these elderly baby boomers.
What
is DHS doing to achieve this goal?
DHS is encouraging more personal savings and use of private financing
options, such as long-term care insurance, providing information and
assistance that allows consumers to make informed choices that meet their
needs and preferences, and targeting public funding to services that support
low-income people in community-based settings so they can avoid nursing home
placement.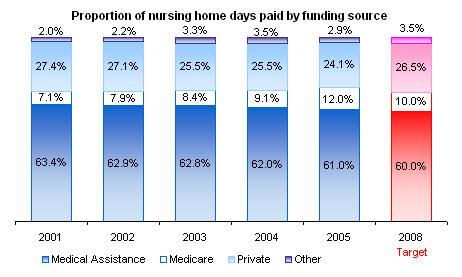
In 2005, DHS began Transform 2010, a project to identify the impacts that
the aging of the state’s population will have and to prepare Minnesota for
this demographic change. DHS has been working for several years on expanding
the financing options that will enable consumers to use their own resources
to pay for their future long-term care needs. The newest option soon to be
available is the Long-Term Care Partnership program. Minnesotans who
purchase certain long-term care insurance policies will be able to protect
more of their assets under this new state plan. The plan is intended to give
people greater control over how they finance their long-term care. DHS also
is helping to redesign long-term care to emphasize home and community-based
services and helping Minnesota communities develop the type of home and
community services their older residents prefer.
 |
 |
|
|
How
is DHS’ progress?
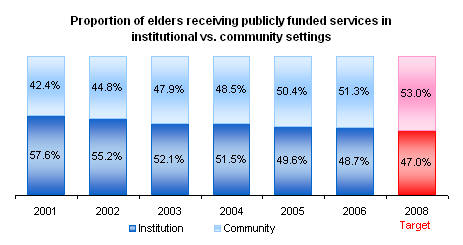
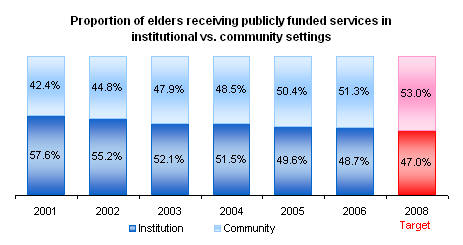
In 2006, 48.7 percent of older Minnesotans needing publicly funded long-term
care services received those services in nursing homes, and 51.3 percent
received services in the community. DHS’ goal is to continue to increase the
proportion of older Minnesotans receiving long-term care services in the
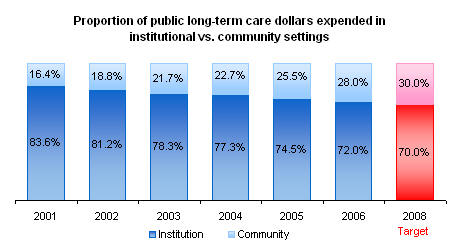
community. 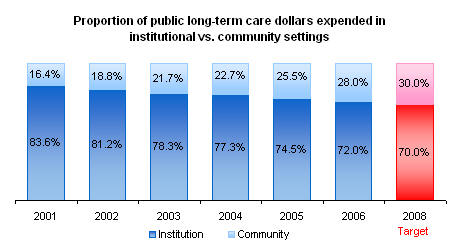 Another goal is to further reduce the proportion of public
funding spent on institutions. In 2006, 72.0 percent of public long-term
care funds for the elderly were spent on nursing home care, and 28.0 percent
of the funds were spent on
community services. Another goal is to further reduce the proportion of public
funding spent on institutions. In 2006, 72.0 percent of public long-term
care funds for the elderly were spent on nursing home care, and 28.0 percent
of the funds were spent on
community services.
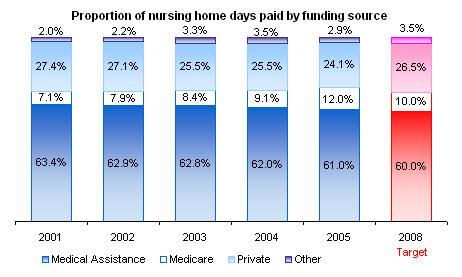
DHS’ long-term strategy is to reduce this reliance on public funding and
increase the proportion of nursing home days paid by private and other
funding. In 2005, Medical Assistance and Medicare paid for 73 percent of
nursing home days, and private and other sources paid for 27 percent.
|
|
|
Goal:
Minnesotans with mental illness will receive timely and needed services in
or near their own communities and will rely less on services in
institutions |
|
Why is this goal important?
Since the late 1980s Minnesota has envisioned serving people with mental
illness in community-based settings rather than large public institutions.
Research also has shown that people with mental illness are better served in
or near their homes as well as near the natural supports of family and
friends, using a wide range of mental health treatment practices that have
proven to be effective. It is estimated that 20 to 30 percent of people in
an institutional (Regional Treatment Center) setting would be better served
in community-based settings, including permanent housing.
|
|
What is DHS doing to achieve this goal?
DHS, counties and other partners are moving mental health services from
state institutions to local communities. An array of community-based
services are being developed by regional planning groups to meet the needs
of adults with mental illness. Among the array of services will be acute
psychiatric inpatient care provided by small state-operated
Community-Behavioral Health Hospitals or community hospital psychiatric
units.
|
|
How is DHS’
progress?
In 2006, 5 percent of people with serious and persistent mental illness
received some or all of their services in an institution. The goal is to
reduce reliance on institutional settings by improving community-based
services.
The average number of annual bed-days for persons treated in an institution
for mental illness in 2006 was 65.3 days. DHS’ goal is to reduce that
average as a measure of
increased access and improvement in community-based services.
In 2006, 11 percent of people discharged from an institution were admitted
to either an institutional or a hospital setting within 30 days of being
discharged. DHS’ goal is to reduce this percentage over time by improving
inpatient treatment and access to community-based services.
|
|
Goal:
More children will live in safe and permanent homes |
|
Why is this goal important?
Every child deserves a safe, loving, permanent home. Children who have their
physical, emotional, and mental health needs met are more successful in
their families, schools, and communities and more likely to become
productive, contributing members of society. Safety and stability are
paramount to achieving the well-being of children. Positive enduring
relationships provide a foundation for successful childhood development and
lifelong self-sufficiency.
The Minnesota Department of Human Services seeks to provide permanent
families for children by supporting parents so that they can safely care for
their children or by finding an alternative permanent family, preferably
with relatives or an adoptive family, to care for children when they cannot
safely remain at home. Recognizing that a disproportionate number of
families of color and American Indian heritage are part of the child welfare
system, the department will strive to ensure there is equity in the access
to and delivery of services for all families, particularly families of color
and American Indian heritage.
|
|
How will this goal be accomplished?
Although the Minnesota Department of Human Services has a good record of
establishing safety and permanency for children who need protection,
opportunities to improve the way government responds are being pursued. The
department is working to provide a continuum of services focused on
prevention and early intervention to ensure that children can remain safely
at home with their parents.
Several key initiatives implemented thus far include:
·
Pursuing Alternative Response
(http://www.iarstl.org),
a strength-based assessment that offers broader services to families
referred to the child protection system
· Working with the courts and counties to improve permanency timelines for
children through the Children’s Justice Initiative
·
 Focusing on permanency for children through the work of the Public/Private
Adoption Initiative, the implementation of The Homecoming Project, the
implementation of Concurrent Permanency Planning, and ongoing collaboration
with stakeholders. Focusing on permanency for children through the work of the Public/Private
Adoption Initiative, the implementation of The Homecoming Project, the
implementation of Concurrent Permanency Planning, and ongoing collaboration
with stakeholders.
While working toward safety and permanency for children, the department has taken
extensive measures to address disparities in the child welfare system by:
·
Implementing the recommendations of the African American Disparities
Advisory Committee
·
Working with the University of Minnesota on two studies to examine
child neglect in and services provided to black families
·
Implementing the recommendations of the American Indian Disparities
Advisory Committee.
|
|
 What
is DHS’ progress to date? What
is DHS’ progress to date?
Recurrence:
The national standard for child maltreatment recurrence is measured after
six months of the first maltreatment determination. Nationally, 93.9 percent
of children served by child protection are not subject to repeat
maltreatment in the six months following an initial report. However,
Minnesota believes it’s important to use a longer period (12 months) in
judging our success. In Minnesota, about 92.5 percent of the children served
by child protection are not subjected to repeat maltreatment in the year
following an initial report (CY2006). We hope to improve this outcome over
the next year.
Results by race and ethnicity.
Timely Reunification: Minnesota has a
very high rate of return
of children to their parents within the first year of out-of-home placement;
in CY2006, 90.4 percent of children returned home in that timeframe.
Results by race and ethnicity.
 |
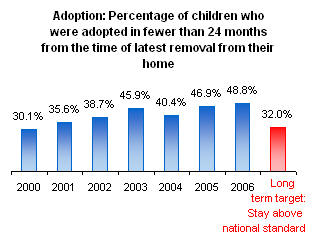 |
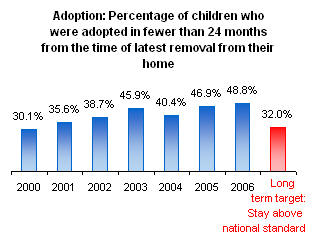
Timely Adoption:
In CY2006,
48.8 percent
of the children under state guardianship who were
adopted that year had their adoptions finalized within two years of their
most recent out-of-home placement. Results by race and ethnicity.
Reentry: 80.9 percent of children entering out-of-home care
in 2006 did not have a prior placement within the previous 12 months.
Results by race and ethnicity. |
|
| |
|
Goal:
Reduce disparities in service access and outcomes |
|
Why is this goal important?
Minnesota leads the nation in providing access to human services and in key
client outcomes. Yet, we lag among certain groups – particularly rural
Minnesotans, people of color, and American Indians. These disparities are
unacceptable. Examples include:
·
 As discussed in the prior goal: “More children will live in safe and
permanent homes,” children of color and American Indian heritage are overrepresented in the
child welfare system. Black and American Indian/Alaska Native children are
about seven times more likely to be determined victims of maltreatment than
white children. As discussed in the prior goal: “More children will live in safe and
permanent homes,” children of color and American Indian heritage are overrepresented in the
child welfare system. Black and American Indian/Alaska Native children are
about seven times more likely to be determined victims of maltreatment than
white children.
·
DHS analyses show there are disparities in outcomes by racial/ethnic and
immigrant status for clients of the Minnesota Family Investment Program, the
state’s primary economic assistance program to help low-income families
become self-sufficient. When controlling for several individual demographic
and county economic characteristics in order to “level the playing field,”
some outcomes were lower than expected for several racial/ethnic groups.
·
More than 90 percent of Minnesotans have health care
coverage, and the state is consistently ranked as one of the “healthiest
states” based on a variety of access and outcome measures. Within this
record, there are gaps in performance. The disparities include: a
comparatively high rate of uninsurance among Hispanics (17.3 percent),
American Indians (16.1 percent) and blacks (15.6 percent). In addition,
children receiving Minnesota Health Care Program benefits have a lower rate
of well-child visits than the commercial managed care population.
|
|
What is DHS doing to achieve this goal?
The department is working to identify gaps, set goals, and implement
targeted, coordinated strategies to reduce disparities and improve outcomes.
DHS will build on efforts under way with counties aimed at reducing
disparities among Minnesota Family Investment Program participants and among
children of color and American Indian heritage receiving health care and
child welfare services. DHS is evaluating where inequities exist at key
decision points when individuals and families come in contact with its services and will implement strategies
so people will experience similar results regardless of their race,
ethnicity, or where they live.
 |
|
How is DHS’ progress?
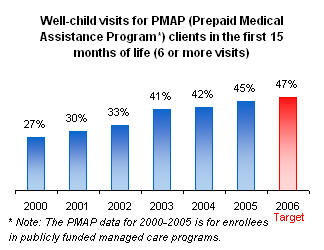
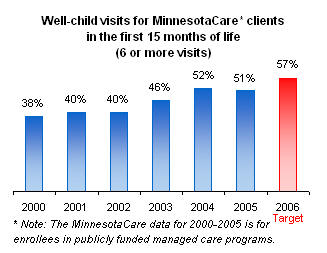
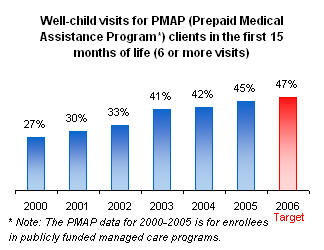
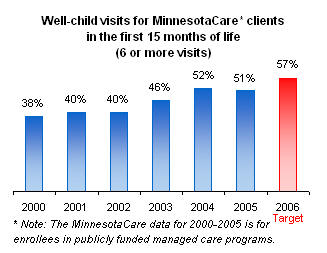
The 2005 data indicates that for children enrolled in the managed care
Prepaid Medical Assistance Programs (PMAP), 45 percent of those in the first
15 months of life received the recommended number of well-child visits for
their age group. The comparable figure for children enrolled in the
MinnesotaCare managed care program is 51 percent. The goal is to increase
these rates. In general, publicly funded managed care programs lag behind
commercial managed care program performance on this measure. In 2005, the
overall figure for managed care plans in Minnesota was 59 percent.
 |
 |
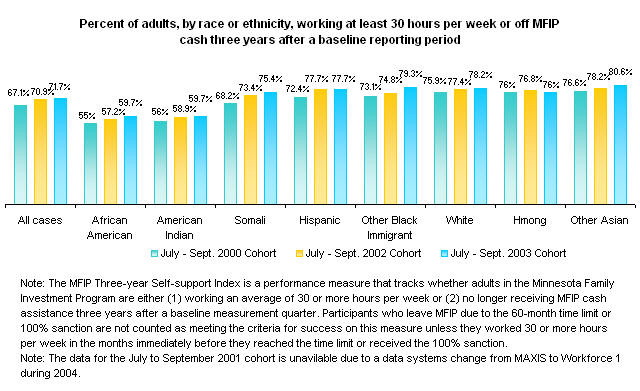
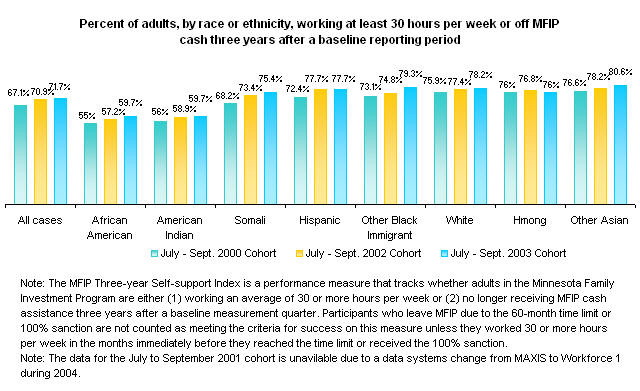
The latest MFIP data indicates that for
the July to September 2006 quarter, almost 71.7 percent of all adults are
working at least 30 hours per week or off MFIP cash assistance three years
after a baseline reporting period, compared with 67.1 percent for the same
quarter in 2003. Outcomes for African American and American Indian adults
also improved over the same period but are not at the same level. The
department has received a multi-year matching grant from the Otto Bremer
Foundation to work with counties in order to further understand and reduce
these disparities in outcomes. For more information about MFIP and
racial/ethnic and immigrant groups see the reports in the
"Welfare Reform Outcomes of Racial/Ethnic
and Immigrant Groups in Minnesota: Racial/Ethnic and Immigrant Studies
(REIS) Series." (http://www.dhs.state.mn.us/main/groups/economic_support/documents/pub/dhs_id_004113.hcsp) |
| |
|
Some images © 2003 www.clipart.com |
|
Last update on
07/24/2007 |
|


 Rising health care costs are a serious problem. While there is no magic
bullet to make the problem go away, the Minnesota Department of Human
Services (DHS) is looking at a number of initiatives that will reduce costs
in both the short and long term.
Rising health care costs are a serious problem. While there is no magic
bullet to make the problem go away, the Minnesota Department of Human
Services (DHS) is looking at a number of initiatives that will reduce costs
in both the short and long term.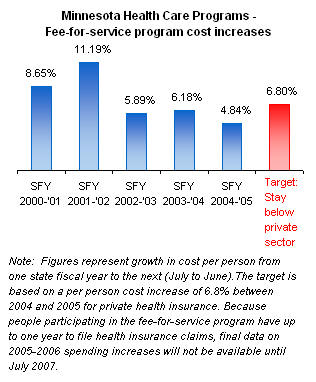

 As the major payer of long-term care services, the state could be
overwhelmed by the cost of long-term care for these elderly baby boomers.
As the major payer of long-term care services, the state could be
overwhelmed by the cost of long-term care for these elderly baby boomers.

 Another goal is to further reduce the proportion of public
funding spent on institutions. In 2006, 72.0 percent of public long-term
care funds for the elderly were spent on nursing home care, and 28.0 percent
of the funds were spent on
community services.
Another goal is to further reduce the proportion of public
funding spent on institutions. In 2006, 72.0 percent of public long-term
care funds for the elderly were spent on nursing home care, and 28.0 percent
of the funds were spent on
community services. 


 Focusing on permanency for children through the work of the Public/Private
Adoption Initiative, the implementation of The Homecoming Project, the
implementation of Concurrent Permanency Planning, and ongoing collaboration
with stakeholders.
Focusing on permanency for children through the work of the Public/Private
Adoption Initiative, the implementation of The Homecoming Project, the
implementation of Concurrent Permanency Planning, and ongoing collaboration
with stakeholders. What
is DHS’ progress to date?
What
is DHS’ progress to date?
 As discussed in the prior goal: “More children will live in safe and
permanent homes,” children of color and American Indian heritage are overrepresented in the
child welfare system. Black and American Indian/Alaska Native children are
about seven times more likely to be determined victims of maltreatment than
white children.
As discussed in the prior goal: “More children will live in safe and
permanent homes,” children of color and American Indian heritage are overrepresented in the
child welfare system. Black and American Indian/Alaska Native children are
about seven times more likely to be determined victims of maltreatment than
white children.